Weight and Foot Problems

Many people are considered to be overweight or obese, which can negatively impact the feet in various ways. Carrying excess weight increases the load on the feet during weight bearing activities, and can lead to pain and injuries that discourage physical activity. Additionally, obesity may raise the risk of chronic diseases such as diabetes, which can harm peripheral circulation and nerve supply in the feet. This issue is not limited to adults. Childhood obesity is a growing concern, with structural and functional changes in the feet that can affect a child's current well being and may persist into adulthood. Common foot complaints related to increased weight include non specific foot pain, tendonitis, plantar fasciitis, and osteoarthritis. It is important to remember that obesity is a complex issue with various contributing factors, including genetics, lifestyle, and environmental influences. Blaming or stigmatizing individuals for their weight can be counterproductive and harmful. Instead, offering support, encouragement, and resources for maintaining a healthy lifestyle can be more effective in addressing both obesity and its related health concerns, including foot problems. If you are overweight and are experiencing foot consequences, it is suggested that you make an appointment with a compassionate podiatrist who can provide you with help in living a healthier lifestyle and relieving your foot pain.
Obesity has become very problematic at this point in time and can have extremely negative effects on the feet. If you’re an obese individual and are concerned about your feet, contact Gregory Rorick, DPM from Rorick Podiatry, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
Since your feet are what support your entire weight when standing, any additional weight can result in pain and swelling. Being overweight is one of the main contributors to foot complications.
Problems & Complications
Extra Weight – Even putting on just a few extra pounds could create serious complications for your feet. As your weight increases, your balance and body will shift, creating new stresses on your feet. This uneven weight distribution can cause pain, even while doing the simplest tasks, such as walking.
Diabetes – People who are overweight are at serious risk of developing type-2 diabetes, which has a drastic impact on the health of your feet. As you get older, your diabetes might worsen, which could lead to loss of feeling in your feet, sores, and bruises. You could also become more prone to various infections.
Plantar fasciitis – Pressure and stress that is placed on muscles, joints, and tendons can trigger plantar fasciitis, which is an inflammation of tissue that forms along the bottom of the foot.
If you have any questions please feel free to contact our office located in New York Mills, Utica, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How Obesity Affects Your Feet
Gaining weight can happen suddenly and at any time. Usually you won’t notice the extra weight until your feet start hurting at the end of the day. This happens as your feet begin adjusting to carrying more weight. Foot swelling and pain are two of the biggest side effects of having gained weight.
Many foot-related problems can occur even after just putting on a few pounds. This includes the body ‘compensating’ by changing the way it moves. You may find yourself putting extra weight on the wrong parts of your feet and even leaning forward a bit. Your feet were designed to carry a healthy, normal body weight. Extra weight places undue stress on them.
Being overweight often causes the development of Type-2 diabetes, causing leg and foot pain. Older people who do not attempt to control their condition can even lose sensation and feeling in their legs and feet. This can lead to the development of small sores that can lead to serious infection.
Extra stress placed on the joints, tendons and muscles in the feet as a result of extra body weight may also cause heel spurs, or plantar fasciitis. Plantar fasciitis is an inflammation of the foot tissue, causing stiffness and pain when walking and climbing stairs. This can usually be relieved by foot stretches and custom made orthotic shoe-inserts.
Problems in the feet triggered by obesity can be treated by paying special attention to footwear. Proper support shoes that allow for good circulation, especially in the arch and ankle, are vital. A podiatrist can help you find what sort of shoe is most suitable for your feet. They can also measure you for special orthotics if necessary.
It could also be high time to start losing weight in order to treat and prevent diabetes as well as other life threatening diseases. Some methods include yoga and water aerobics, which benefit your entire body without placing stress on your feet. Don’t risk losing your feet by losing interest in them. Take care of your feet and your body, as they deserve the very best.
Morton’s Neuroma Symptoms and Treatment
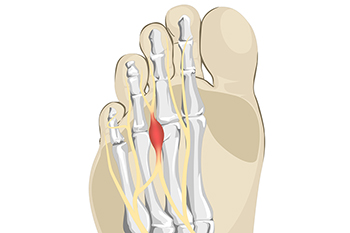
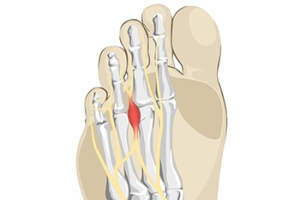
A network of plantar digital nerves in the feet supply sensory signals to the forefoot and toes. Problems arise when these nerves encounter compression, which can occur when the toes are consistently pressed together, effectively obstructing the pathway for these nerves. Such compression often causes a condition known as Morton's neuroma. This may be the result of wearing high heels that force body weight onto the ball of the foot. When the plantar nerves become entrapped, their ability to efficiently transmit signals is affected. This leads to symptoms, including sharp, burning, or tingling sensations in the forefoot and toes. Individuals with Morton's neuroma may also experience numbness or the feeling of having a pebble or foreign object in their shoe. Morton's neuroma can be effectively managed in several ways. Start with footwear that has cushioning and provides adequate room for the toes. Custom orthotics can also help alleviate pressure on the affected area. In more severe cases, corticosteroid injections or surgical intervention may be recommended. If you suspect you are suffering from Morton's neuroma, it's suggested that you make an appointment with a podiatrist for a diagnosis and treatment plan tailored to your needs.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Gregory Rorick, DPM of Rorick Podiatry, PC. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in New York Mills, Utica, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Are Bunions Affecting Your Everyday Life?
Causes and Symptoms of Bunions

A bunion is a common foot deformity that affects the joint at the base of the big toe. This condition occurs when the big toe deviates outward, causing the joint to protrude and creating a visible bump on the side of the foot. Bunions typically develop over time due to a variety of factors. Genetics plays a significant role, as the shape and structure of your foot can predispose you to bunions. Wearing ill-fitting shoes, especially those with narrow-toe boxes or high heels, can exacerbate the condition. Additionally, inflammatory joint conditions like arthritis may contribute to bunion formation. The symptoms of a bunion can range from mild to severe. Common signs include pain, swelling, redness, and tenderness around the affected joint. Over time, the big toe may angle towards the other toes, causing discomfort and difficulty finding well-fitting shoes. The skin over the bunion may become thickened and calloused. For some individuals, bunions can restrict their daily activities and lead to further foot problems if left untreated. If you have developed a bunion, it is strongly suggested that you consult a podiatrist who can offer you relief and treatment options that are right for you.
If you are suffering from bunion pain, contact Gregory Rorick, DPM of Rorick Podiatry, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in New York Mills, Utica, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
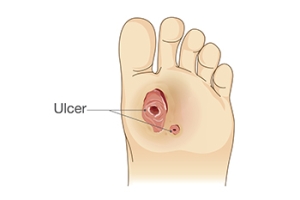
A Guide to Caring for Diabetic Foot Ulcers
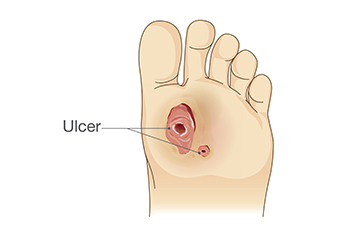
Diabetic foot ulcers are common among those with diabetes, requiring vigilant wound care to prevent complications and promote healing. These ulcers often develop due to reduced blood circulation and nerve damage in the feet, making them slower to heal and more susceptible to infection. The key to managing diabetic foot ulcers lies in meticulous care. This can begin by keeping the wound clean to prevent infections. Regularly change dressings and use prescribed topical antibiotics if necessary. Removing pressure from the affected foot and using special footwear may help to redistribute weight. Monitor blood sugar levels because high glucose levels can impede the healing process. Consulting a podiatrist is essential for proper wound assessment and care. They may recommend advanced wound dressings, debridement, or surgical interventions if the ulcer is severe. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can help manage this condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Gregory Rorick, DPM from Rorick Podiatry, PC. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in New York Mills, Utica, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Causes and Treatment of Foot Neuropathy

Neuropathy in the feet is a complex and often debilitating condition that affects millions of people worldwide. It refers to damage or dysfunction of the peripheral nerves, leading to a range of distressing symptoms. These can include numbness, tingling, and burning sensations, in addition to sharp pains in the feet. The causes of neuropathy in the feet are diverse, with diabetes being a leading factor. Other potential triggers include alcohol abuse, certain medications, and infections. Additionally, autoimmune diseases and traumatic injuries can contribute to developing neuropathy. Early detection is important, as untreated neuropathy can lead to severe complications, such as foot ulcers. Effective treatment approaches depend on the underlying cause. Managing blood sugar levels and lifestyle modifications are essential for reducing the effects of diabetic neuropathy. Medication, such as pain relievers, may be prescribed to alleviate symptoms. Early intervention and a comprehensive treatment plan can help manage neuropathy, improving the quality of life for those affected. If you are affected by foot neuropathy, it is strongly suggested that you visit a podiatrist who can guide you toward effective relief and treatment options.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Gregory Rorick, DPM from Rorick Podiatry, PC. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in New York Mills, Utica, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.