June 2021
Common Uses for Orthotics
 Orthotics are inserted into the shoes and are worn to correct issues with foot alignment or relieve pressure for other foot related issues. Orthotics can also help with problems like knee pain and lower back pain. They can be designed to take stress off of certain areas of the feet, and they can also help support and align the feet properly. Orthotics can be made custom by laser scanning the foot, by using a foam box, or by making a plaster cast. Orthotics can be used to delay surgery, particularly when a child needs to wait for their growth plates to close or for their bones to grow to the needed size. Orthotics may also be used post-surgery to help alleviate pain. If you believe orthotics are right for you, consulting with a podiatrist is suggested.
Orthotics are inserted into the shoes and are worn to correct issues with foot alignment or relieve pressure for other foot related issues. Orthotics can also help with problems like knee pain and lower back pain. They can be designed to take stress off of certain areas of the feet, and they can also help support and align the feet properly. Orthotics can be made custom by laser scanning the foot, by using a foam box, or by making a plaster cast. Orthotics can be used to delay surgery, particularly when a child needs to wait for their growth plates to close or for their bones to grow to the needed size. Orthotics may also be used post-surgery to help alleviate pain. If you believe orthotics are right for you, consulting with a podiatrist is suggested.
If you are having discomfort in your feet and would like to try orthotics, contact Gregory Rorick, DPM from Rorick Podiatry, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in New York Mills, Utica, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Orthotics
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.
Achilles Tendonitis Can Turn Into Tendonosis
 The Achilles tendon is a thick band of fibrous tissue located at the back of the lower leg. It connects the calf muscle to the heel bone and allows us to walk by raising the heel off of the ground. Repetitive stress placed on this tendon during activities such as running, playing high impact sports, and working on your feet can cause the tendon to become injured. Initially, the Achilles tendon may become inflamed in a condition known as Achilles tendonitis. An inflamed Achilles tendon can be painful, tender, and stiff. If left untreated, Achilles tendonitis could become chronic and lead to a degeneration of the tendon known as Achilles tendonosis. This condition makes the tendon lose its organized structure and makes it more likely to develop microscopic tears that cause chronic pain and may restrict mobility. Achilles tendonosis can also make a full rupture more likely. If you experience pain in your calf muscles, it is strongly suggested that you seek the care of a podiatrist who can diagnose and treat your condition and prevent further injury.
The Achilles tendon is a thick band of fibrous tissue located at the back of the lower leg. It connects the calf muscle to the heel bone and allows us to walk by raising the heel off of the ground. Repetitive stress placed on this tendon during activities such as running, playing high impact sports, and working on your feet can cause the tendon to become injured. Initially, the Achilles tendon may become inflamed in a condition known as Achilles tendonitis. An inflamed Achilles tendon can be painful, tender, and stiff. If left untreated, Achilles tendonitis could become chronic and lead to a degeneration of the tendon known as Achilles tendonosis. This condition makes the tendon lose its organized structure and makes it more likely to develop microscopic tears that cause chronic pain and may restrict mobility. Achilles tendonosis can also make a full rupture more likely. If you experience pain in your calf muscles, it is strongly suggested that you seek the care of a podiatrist who can diagnose and treat your condition and prevent further injury.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Gregory Rorick, DPM of Rorick Podiatry, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in New York Mills, Utica, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
What Does Plantar Fasciitis Feel Like?
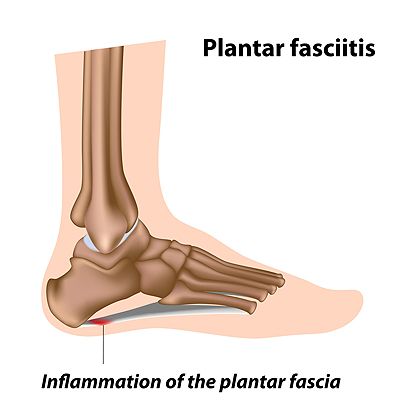 Plantar fasciitis is a common foot problem in which the ligament that runs along the bottom of the foot is injured and becomes inflamed, leading to foot pain. More specifically, plantar fasciitis tends to cause pain in the heel and arch of the foot. In its initial stages, this condition can make you feel an uncomfortable sensation under your heel, as if you have a lump there. The heel may feel tender when you take your first steps after a long period of rest, but pain usually subsides as you get moving about your day. Over time, however, the pain and tenderness may stay with you longer. You might feel stabbing or needle-like pain in your heels. In the most advanced stages of plantar fasciitis, the pain becomes constant and interferes with your daily activities. If you suspect you may have plantar fasciitis, please seek the care of a podiatrist.
Plantar fasciitis is a common foot problem in which the ligament that runs along the bottom of the foot is injured and becomes inflamed, leading to foot pain. More specifically, plantar fasciitis tends to cause pain in the heel and arch of the foot. In its initial stages, this condition can make you feel an uncomfortable sensation under your heel, as if you have a lump there. The heel may feel tender when you take your first steps after a long period of rest, but pain usually subsides as you get moving about your day. Over time, however, the pain and tenderness may stay with you longer. You might feel stabbing or needle-like pain in your heels. In the most advanced stages of plantar fasciitis, the pain becomes constant and interferes with your daily activities. If you suspect you may have plantar fasciitis, please seek the care of a podiatrist.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Gregory Rorick, DPM from Rorick Podiatry, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in New York Mills, Utica, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Wounds That Don't Heal Need to Be Checked
Understanding Corns and Calluses
Corns and Calluses are both hardened layers of thickened skin that develop because of friction. Both ailments are typically found on the feet and may be unsightly. Although they have similarities, corns and calluses are different from each other.
Some causes of corns and calluses may be wearing ill-fitting shoes and not wearing socks. If you wear tight shoes, your feet will constantly be forced to rub against the shoes, causing friction. If you fail to wear socks, you are also causing your feet to endure excess friction.
There are some signs that may help you determine whether you have one of these two conditions. The first symptom is a thick, rough area of skin. Another common symptom is a hardened, raised bump on the foot. You may also experience tenderness or pain under the skin in addition to flaky, dry, or waxy skin.
There are also risk factors that may make someone more prone to developing corns and calluses. If you are already dealing with bunions or hammertoe, you may be more vulnerable to having corns and calluses as well. Other risk factors are foot deformities such as bone spurs, which can cause constant rubbing inside the shoe.
Corns tend to be smaller than calluses and they usually have a hard center surrounded by inflamed skin. They also tend to develop on the parts of the body that don’t bear as much weight such as the tops and sides of toes. Corns may also be painful for those who have them. On the other hand, calluses are rarely painful. These tend to develop on the bottom of the feet and may vary in size and shape.
Fortunately, most people only need treatment for corns and calluses if they are experiencing discomfort. At home treatments for corns and calluses should be avoided, because they will likely lead to infection. If you have either of these ailments it is advised that you consult with your podiatrist to determine the best treatment option for you.
Types of Corns and Calluses
 When walking or standing for long periods of time, certain areas of the skin on the feet thicken to help withstand pressure. These areas of thickness are either corns or calluses that work as a protective measure when the skin rubs on the bone, shoe or the ground. Calluses are larger, more irregularly shaped areas of hardened skin on the foot that usually indicate an issue such as a bone deformity, poor walking style, or poor footwear. Corns are much smaller and have a central core. There are five main types of corns that can develop on the feet. Hard corns are concentrated to the size of a pea, and soft corns develop similarly and usually appear when the skin is moist from sweat or in between the toes. A seed corn is very tiny and can occur by itself or as a cluster. Vascular corns contain nerve fibers and blood vessels and are very painful. Fibrous corns attach to deeper tissues and tend to last a long time on the foot. If you have a corn or callus that is irritating your foot, consulting with a podiatrist is suggested.
When walking or standing for long periods of time, certain areas of the skin on the feet thicken to help withstand pressure. These areas of thickness are either corns or calluses that work as a protective measure when the skin rubs on the bone, shoe or the ground. Calluses are larger, more irregularly shaped areas of hardened skin on the foot that usually indicate an issue such as a bone deformity, poor walking style, or poor footwear. Corns are much smaller and have a central core. There are five main types of corns that can develop on the feet. Hard corns are concentrated to the size of a pea, and soft corns develop similarly and usually appear when the skin is moist from sweat or in between the toes. A seed corn is very tiny and can occur by itself or as a cluster. Vascular corns contain nerve fibers and blood vessels and are very painful. Fibrous corns attach to deeper tissues and tend to last a long time on the foot. If you have a corn or callus that is irritating your foot, consulting with a podiatrist is suggested.
If you have any concerns regarding your feet and ankles, contact Gregory Rorick, DPM of Rorick Podiatry, PC. Our doctor will treat your foot and ankle needs.
Corns: What Are They? and How Do You Get Rid of Them?
Corns can be described as areas of the skin that have thickened to the point of becoming painful or irritating. They are often layers and layers of the skin that have become dry and rough, and are normally smaller than calluses.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as wearing:
- Well-fitting socks
- Comfortable shoes that are not tight around your foot
- Shoes that offer support
Treating Corns
Treatment of corns involves removing the dead skin that has built up in the specific area of the foot. Consult with Our doctor to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our office located in New York Mills, Utica, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What to Do About Sweaty Feet
 Excessive sweating, also known as hyperhidrosis, can affect any part of the body. However, the feet have more sweat glands per inch than any other part of the body. While most of us have dealt with sweaty feet every so often, for some people sweaty feet can be a constant problem. This constant sweat can be uncomfortable, embarrassing, and impact daily life. Overly sweaty feet are usually a result of overactive sweat glands that can are caused by genetics or changing hormone levels in the body. The first step to dealing with sweaty feet is to focus on proper foot hygiene, this includes washing the feet, using absorbent foot powder, and rotating the shoes that are worn each day. Patients who continue to struggle with overly sweaty feet should consult with a podiatrist to find a proper treatment method.
Excessive sweating, also known as hyperhidrosis, can affect any part of the body. However, the feet have more sweat glands per inch than any other part of the body. While most of us have dealt with sweaty feet every so often, for some people sweaty feet can be a constant problem. This constant sweat can be uncomfortable, embarrassing, and impact daily life. Overly sweaty feet are usually a result of overactive sweat glands that can are caused by genetics or changing hormone levels in the body. The first step to dealing with sweaty feet is to focus on proper foot hygiene, this includes washing the feet, using absorbent foot powder, and rotating the shoes that are worn each day. Patients who continue to struggle with overly sweaty feet should consult with a podiatrist to find a proper treatment method.
If you are suffering from hyperhidrosis contact Gregory Rorick, DPM of Rorick Podiatry, PC. Our doctor can provide the care you need to attend to all of your foot and ankle needs.
Hyperhidrosis of the Feet
Hyperhidrosis is a rare disorder that can cause people to have excessive sweating of their feet. This can usually occur all on its own without rigorous activity involved. People who suffer from hyperhidrosis may also experience sweaty palms.
Although it is said that sweating is a healthy process meant to cool down the body temperature and to maintain a proper internal temperature, hyperhidrosis may prove to be a huge hindrance on a person’s everyday life.
Plantar hyperhidrosis is considered to be the main form of hyperhidrosis. Secondary hyperhidrosis can refer to sweating that occurs in areas other than the feet or hands and armpits. Often this may be a sign of it being related to another medical condition such as menopause, hyperthyroidism and even Parkinson’s disease.
In order to alleviate this condition, it is important to see your doctor so that they may prescribe the necessary medications so that you can begin to live a normal life again. If this is left untreated, it is said that it will persist throughout an individual’s life.
A last resort approach would be surgery, but it is best to speak with your doctor to find out what may be the best treatment for you.
If you have any questions please feel free to contact our office located in New York Mills, Utica, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.